
Xiaoyue Xu (Luna), UNSW Sydney; Alta Schutte, UNSW Sydney, and Bruce Neal, George Institute for Global Health
One in three Australian adults has high blood pressure (hypertension). Excess salt (sodium) increases the risk of high blood pressure so everyone with hypertension is advised to reduce salt in their diet.
But despite decades of strong recommendations we have failed to get Australians to cut their intake. It’s hard for people to change the way they cook, season their food differently, pick low-salt foods off the supermarket shelves and accept a less salty taste.
Now there is a simple and effective solution: potassium-enriched salt. It can be used just like regular salt and most people don’t notice any important difference in taste.
Switching to potassium-enriched salt is feasible in a way that cutting salt intake is not. Our new research concludes clinical guidelines for hypertension should give patients clear recommendations to switch.
What is potassium-enriched salt?
Potassium-enriched salts replace some of the sodium chloride that makes up regular salt with potassium chloride. They’re also called low-sodium salt, potassium salt, heart salt, mineral salt, or sodium-reduced salt.
Potassium chloride looks the same as sodium chloride and tastes very similar.
Potassium-enriched salt works to lower blood pressure not only because it reduces sodium intake but also because it increases potassium intake. Insufficient potassium, which mostly comes from fruit and vegetables, is another big cause of high blood pressure.
What is the evidence?
We have strong evidence from a randomised trial of 20,995 people that switching to potassium-enriched salt lowers blood pressure and reduces the risks of stroke, heart attacks and early death. The participants had a history of stroke or were 60 years of age or older and had high blood pressure.

An overview of 21 other studies suggests much of the world’s population could benefit from potassium-enriched salt.
The World Health Organisation’s 2023 global report on hypertension highlighted potassium-enriched salt as an “affordable strategy” to reduce blood pressure and prevent cardiovascular events such as strokes.
What should clinical guidelines say?
We teamed up with researchers from the United States, Australia, Japan, South Africa and India to review 32 clinical guidelines for managing high blood pressure across the world. Our findings are published today in the American Heart Association’s journal, Hypertension.
We found current guidelines don’t give clear and consistent advice on using potassium-enriched salt.
While many guidelines recommend increasing dietary potassium intake, and all refer to reducing sodium intake, only two guidelines – the Chinese and European – recommend using potassium-enriched salt.
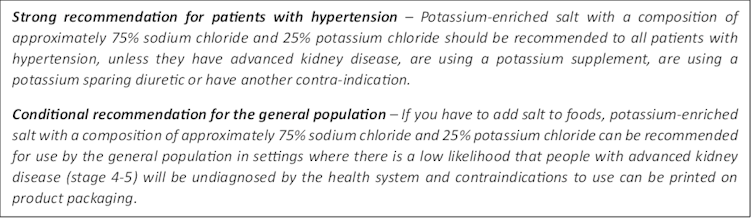
To help guidelines reflect the latest evidence, we suggested specific wording which could be adopted in Australia and around the world:
Why do so few people use it?
Most people are unaware of how much salt they eat or the health issues it can cause. Few people know a simple switch to potassium-enriched salt can help lower blood pressure and reduce the risk of a stroke and heart disease.
Limited availability is another challenge. Several Australian retailers stock potassium-enriched salt but there is usually only one brand available, and it is often on the bottom shelf or in a special food aisle.
Potassium-enriched salts also cost more than regular salt, though it’s still low cost compared to most other foods, and not as expensive as many fancy salts now available.

A 2021 review found potassium-enriched salts were marketed in only 47 countries and those were mostly high-income countries. Prices ranged from the same as regular salt to almost 15 times greater.
Even though generally more expensive, potassium-enriched salt has the potential to be highly cost effective for disease prevention.
Preventing harm
A frequently raised concern about using potassium-enriched salt is the risk of high blood potassium levels (hyperkalemia) in the approximately 2% of the population with serious kidney disease.
People with serious kidney disease are already advised to avoid regular salt and to avoid foods high in potassium.
No harm from potassium-enriched salt has been recorded in any trial done to date, but all studies were done in a clinical setting with specific guidance for people with kidney disease.
Our current priority is to get people being managed for hypertension to use potassium-enriched salt because health-care providers can advise against its use in people at risk of hyperkalemia.
In some countries, potassium-enriched salt is recommended to the entire community because the potential benefits are so large. A modelling study showed almost half a million strokes and heart attacks would be averted every year in China if the population switched to potassium-enriched salt.
What will happen next?
In 2022, the health minister launched the National Hypertension Taskforce, which aims to improve blood pressure control rates from 32% to 70% by 2030 in Australia.
Potassium-enriched salt can play a key role in achieving this. We are working with the taskforce to update Australian hypertension management guidelines, and to promote the new guidelines to health professionals.
In parallel, we need potassium-enriched salt to be more accessible. We are engaging stakeholders to increase the availability of these products nationwide.
The world has already changed its salt supply once: from regular salt to iodised salt. Iodisation efforts began in the 1920s and took the best part of 100 years to achieve traction. Salt iodisation is a key public health achievement of the last century preventing goitre (a condition where your thyroid gland grows larger) and enhancing educational outcomes for millions of the poorest children in the world, as iodine is essential for normal growth and brain development.
The next switch to iodised and potassium-enriched salt offers at least the same potential for global health gains. But we need to make it happen in a fraction of the time.![]()
Xiaoyue Xu (Luna), Scientia Lecturer, UNSW Sydney; Alta Schutte, SHARP Professor of Cardiovascular Medicine, UNSW Sydney, and Bruce Neal, Executive Director, George Institute Australia, George Institute for Global Health
This article is republished from The Conversation under a Creative Commons license. Read the original article.